Operation of an alternate care facility in Seoul, Korea: Responding to the third wave of COVID-19 pandemic
Article information
Abstract
The third wave of the COVID-19 outbreak, in December 2020, overwhelmed the Korean healthcare system. In particular, the medical demand of residents in long-term care facilities, homeless shelters, group homes, and detention facilities surged. In this study, we described the experience from development and operation of an alternate care facility (ACF) against the COVID-19 pandemic. In this study, we describe our implementation strategy, including the layout plan, adequate staffing, admission criteria, and patient flow. Using the context of the existing guidelines and literature in the planning and construction process, the differences from the preceding alternative treatment facilities to respond to COVID-19 were also described. Under the time pressure, the old buildings used as office spaces by the US armies were converted into a 107-bed hospital that met infection prevention and clinical care standards. Since these hospitals were dedicated to caring for the patients with COVID-19, multiple challenges were posed to the standards of infection prevention and control, and patient care and safety. The approaches described here provide a potential roadmap for decision makers, who are coping with medical surges as a result of the current and potential future pandemics by implementing an ACF.
INTRODUCTION
In response of the COVID-19 pandemic, several types of alternative care facility (ACFs) were introduced worldwide [1-5]. The characteristics of these ACFs vary depending on the size of the outbreak, local context and resources, and the underlying healthcare system. However, their common objective was to provide essential capacity to cope with the demands of the COVID-19 pandemic [6].
Korea experienced its first wave of the COVID-19 pandemic between February and March 2020 [7]. In the early stages of the first wave, the Korean government hospitalized all laboratory-confirmed patients with COVID-19 at nationally-designated hospitals to prevent the spread of infection [8]. However, as the number of patients exploded, beds in nationally-designated hospitals across the country were saturated. In Daegu, a hotspot area of the first wave, 741 new cases were reported on February 29, and the local healthcare system was overwhelmed by patient surge. More than 2,000 patients awaited hospitalization, three of whom died at home [9]. To respond the demands of the first wave, a temporary isolation facility for COVID-19 patients with minimal symptoms called community treatment center (CTC) was introduced. Several studies were published on the operational experience of CTC and the characteristics of patients admitted to CTC [8, 10-12].
Up until the third wave in winter, medical capacity, supplemented by the CTCs, seemed sufficient to cater to the needs. However, when long-term care facilities became heavily affected, it was evident that CTCs were insufficient. Although young and low-risk patients could be quickly accommodated in CTCs, high-risk patients in need of serious medical attention had to wait at home, due to the medical surges in hospitals. A minimum of 66 patients died or became critically ill, while waiting at home for 8 weeks during the winter epidemic. Simultaneously, a large-clustered infection developed in the detention facility, where 1,203 of the 3,290 detainees (42.9%) were infected as of January 20 [13]. For security reasons, detainees could not be admitted to hospitals or accommodated in CTCs. This has limited vulnerable populations from receiving adequate medical care in a timely manner and has boosted transmission within the facility.
In this context, the National Medical Center (NMC) decided to establish an ACF, in collaboration with the Korean government, to guarantee timely access and quality care beyond the capability of CTCs, for vulnerable population, either medically or socially. The NMC is a public hospital with 480 acute beds in Seoul, Korea. As a designated hospital for infectious diseases, it provides specialized care to COVID-19 patients transferred from all over the country as well as around Seoul metropolitan city. To this end, NMC operates an exclusive COVID-19 isolation wards with 50 beds and an intensive care unit with 30 beds. In addition, the NMC established an ACF in a former US Army Corps of Engineers Far East District (namely, the NMC-FED) camp site, next to the NMC main campus, in partnership with the Ministry of National Defense and Ministry of Health and Welfare. The purpose of this study is to describe the operation strategy and patient management of the ACF operated by NMC during the third wave of the COVID-19 pandemic in Seoul metropolitan city.
METHODS
Study design and data collection
This is a retrospective, single-center study, including qualitative and quantitative analysis. For qualitative analysis, information was obtained from operational minutes, building service drawings, and site visits. For quantitative analysis, we reviewed the electronic medical record of patients admitted to the NMC-FED between January 19 and March 31, 2021. Through a retrospective medical records review, the following information was extracted using a standardized data collection form: patient demographics, the route of admission, symptoms on admission, comorbidities, medical management during the NMC-FED stay, and the route of discharge. The end point of observation was April 25, 2021. All data were double-checked by two physicians and a third researcher adjudicated any difference in interpretation between the two primary reviewers.
Data analysis
The quantitative data were analyzed using descriptive statistical methods. Baseline patient characteristics, treatments, and clinical outcome were presented as frequencies with percentages for categorical variables, and as the median with interquartile range (IQR; 25th, 75th percentiles) for continuous variables.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of the National Medical Center (NMC-2021-04-031); a waiver of informed consent was obtained for the use of the retrospective data.
RESULTS
Facility layout
Five two-story wooden buildings, used as office spaces by the US armies up until 5 years ago Since these buildings were not designed for patient care, their transformation into care facilities involved multiple issues: layout planning, clinical care flow, infection prevention and control, adequate staffing, and other essential services.
On January 18, 2021, after 18 days of construction, the old buildings were converted into a 107-bed hospital that met infection prevention and clinical care standards, by a local construction company under the leadership of the NMC-FED construction team. The NMC-FED consisted of an emergency intensive care unit, three isolation wards, and annexed buildings for staff respite (Figure 1).
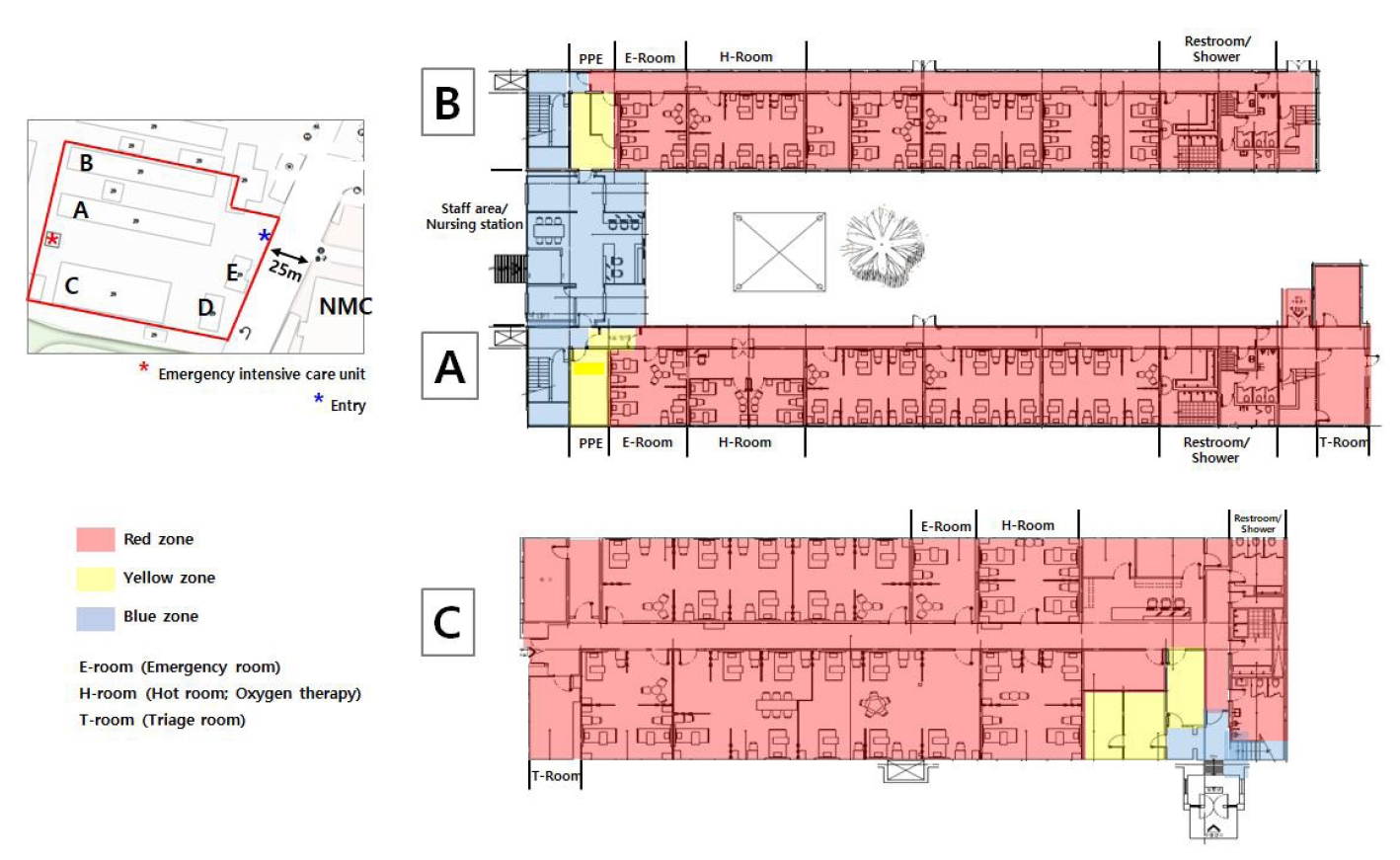
The NMC-FED locations and schematic layout.
The NMC-FED is located next to the NMC main hospital. The facility consisted of five buildings (A–E), of which A, B, and C were designed as hospital wards and D and E were remodeled as a stock room and as a staff office, respectively. The hospital wards were divided into three zones: (1) the red zone for patient care including E-room, H-room, and T-room, (2) the yellow zone for donning/doffing PPEs, and (3) the blue zone - a clean area.
PPE = personal protective equipment
Each isolation ward had an emergency room (E-room) and hot room (H-room) as per their proximity to the nursing station (Figure 1). The E-room was designated to patients staying temporarily, in the event of unexpected critical conditions, before their transfer to the emergency intensive care unit or the main hospital. The H-room was for patients who needed oxygen supplement therapy or close monitoring. The triage spaces (T-room) were made in the A and C wards. The emergency intensive care unit was located immediately after the isolation wards and prepared as a contingency measure; it was negatively pressured and equipped with medical devices and medications for emergency airway management (Figure 2D). Lifts were installed outside the A and B wards, because the old structures had no elevator system.

Zones of NMC-FED.
(A) The exterior of the NMC-FED, as seen from the main gate. (B) The red zone (red line is marked on the wall) is separated from the blue zone by the yellow zone, which can only be accessed by an identification card (in a fire emergency, the digital lock will be deactivated automatically). (C) The E-room is equipped with a negative pressure machine for aerosol-generating procedure. (D) The emergency intensive care unit is prepared as a contingency measure, right next to the patient wards.
Staffing
A typical inpatient unit team consisted of physicians, nurses, and ancillary staff (i.e., for cleaning and meal services). Physicians and nurses were recruited from the Association of Physicians for Humanism, a volunteer organization of physicians, and the Korean Nurses Association, respectively, with the help of the Ministry of Health and Welfare, to ensure a minimum of two physicians per duty and a ratio of three nurses for every 20 patients. The staff received 3 weeks of training for: PPE donning/doffing standards, infection control, safety, patient care, and emergency response. At the end of training, an on-site simulation was conducted for three different scenarios: patient admission; usual discharge; and transfer to the main hospital due to COVID-19 aggravation, emergency situation development, and cardiac arrest. Previous studies suggested that these scenario-based simulations and debriefing play a critical role in actualizing the functioning of the system [14]. A certified pulmonologist was appointed as the clinical director for the NMC-FED, responsible for supervision and capable of allocating on-site and off-site safety resources. The nursing director assigned bed and managed unit-to-unit transfers and worked in close collaboration with the referral center of the NMC main hospital. In the patient care area, staff communicated using a two-way radio system, and all radio communications were monitored by the clinical director.
Admission criteria and patient care
The NMC-FED was designed to provide low-level care for COVID-19 patients with mild to moderate illnesses, who needed to be closely monitored and treated for underlying medical conditions (Table 1). In the admission stage, physicians carefully evaluated patients as per the admission criteria in the T-room; those who did not meet these criteria—those in need of high flow oxygen therapy, extensive nursing care, or assistance with living activities—were referred to the NMC main hospital.
Patients were admitted with their own medicines for the initial 5 days to ensure patient safety and sufficient time for stocking patient-specific medications in the pharmacy; they were verified by a pharmacist in the admission stage. The medicine stock was monitored in real time and medicines were supplied via a courier, twice a day, by the pharmacy staff from the main hospital. Portable oxygen tanks were stored on-site for E-room and H-room patients, requiring oxygen therapy. Similarly, portable monitoring devices—electrocardiograms, electro manometers, and glucometers—were equipped in the wards for diagnostics and testing. Laboratory tests were performed by delivering specimens to the NMC main hospital laboratories. If necessary for radiologic examination, patients were transported to the NMC radiology department. All diagnostic values and images were standardly reported in the NMC electronic medical records system, which the medical staff of the NMC-FED had access to, including physician order entry and laboratory results. Therefore, continuity of care was guaranteed, upon the transfer of a patient from the NMC main hospital.
Discharge criteria were defined in advance: 1) 10 days after the onset of symptom, 2) no fever for at least 24 hours without the use of antipyretics, and 3) improvement of other respiratory symptoms. On the other hand, patients were transferred to the NMC main hospital when: COVID-19 symptoms were aggravated and required high-flow oxygen therapy; significant medical incidents such as cerebrovascular accident or fracture caused by a fall, or emergency evacuation situations such as cardiac arrest occurred. Upon recognizing any of these conditions, the patient was moved to the E-room of the NMC-FED for assessment or emergency care, and if necessary, was subsequently transferred to the NMC main hospital. Moreover, in the event of an emergency, the rapid response team of the NMC was summoned to the NMC-FED.
Facility Operation
The general director of NMC-FED, who was also the vice president of the NMC main hospital, led construction team during the planning and construction phase. This team was comprised of head staff in each area of expertise—planning and coordination, human resources, medical information, facilities and equipment, logistics, medical care, nursing, pharmacy, nutrition, and security.
Once the NMC-FED was functional, a clinical director and a nursing director were appointed from among the physician volunteers and the chief nurses of the NMC main hospital, respectively. Additionally, infectious disease specialists and pulmonologists, from the NMC main hospital, performed back-up duty for the NMC-FED. Nonclinical issues, regarding the functioning and service provision, were reported to the nursing director, who coordinated with the NMC administration office.
Several measures were also taken to reduce airborne infection because the entire building could not be pressured negatively. Each room of patients equipped with an air-conditioning and heating facility, was ventilated naturally every 4 hours and their beds were spaced more than 2 meters apart using a physical barrier. In addition, a portable negative pressure machine was attached in each E-room (Figure 2C).
In order to endure security and safety of patients and staff, a closed-circuit television monitoring system was installed, and the guards regularly patrolled the blue zone of the isolation wards. Moreover, security personnel were stationed at the main gate to inspect the visitors.
Patients
Between January 19 and March 31, 2021, a total of 141 patients with COVID-19 were admitted to NMC-FED. The median age of patients was 56 years (IQR 38-65) and, 63 (42.3%) patients were ≥ 60 years of age. With respect to social vulnerability, 33 (23.4%) patients were foreign nationals and 23 (16.3%) patients were homeless, respectively. Both of groups could not be admitted to regional hospitals nor accommodated to CTCs because they had no residential address for hospital allocation and had difficulties in communication by telemedicine. Among 141 patients, 130 (92.2%) patients were admitted directly to NMC-FED, 9 (6.4%) patients were transferred from outside hospital or CTC, and 2 (1.4%) patients were moved from main NMC ward. On the day of admission, almost half of patients (n = 68 [48.2%]) had body temperature over 37.8°C and 14 (9.9%) patients complained of shortness of breath, whereas 28 (19.9%) patients presented none of COVID-19 related symptoms. Hypertension (n = 48 [34.0%]) and diabetes (n = 21 [14.9%]) were the most common comorbidities. Eleven (7.8%) patients had a major psychiatric disorder (Table 2).
Table 3 showed medical management, length of stay, and outcome of patients admitted to NMC-FED. Low flow oxygen therapy was provided to 17 (12.1%) patients and antiviral agents were administered to 4 (2.8%) out of 141 patients: 2 (1.4%) patients received remdesivir, and 2 (1.4%) patients received monoclonal antibody, respectively. The median length of stay (LOS) was 10 days (IQR 7-11). While 117 patients (83.0%) were discharged to home, 22 (15.6%) patients required a transfer to CTCs (n = 3 [2.1%]) or other hospitals (n = 2 [1.4%]) or main NMC ward (n = 17 [12.1%]), respectively. No patients required intubation prior to transfer. A detailed clinical characteristics of transferred patients is presented in Supplement table 1.
Challenges and implemented solutions
The NMC-FED had converted old wooden buildings into functional hospitals dedicated to caring for the patients with COVID-19, under tremendous time pressure. Accordingly, hospitals were, multiple challenges were posed to the standards of infection prevention and control, and patient care and safety. The NMC-FED tried to develop and implement solutions for these challenges, as presented in Table 4.
DISCUSSION
The ACF model can be categorized into three groups: 1) the non-acute care model, which is focused on capacity building (i.e., increasing beds). This type of facility provides ambulatory (level 5) and minor acuity care (level 4) to asymptomatic and/or mild to moderately symptomatic patients; these patients may require low-flow oxygen therapy, but not extensive nursing care or living assistance. 2) the hybrid care model refers to building capability in addition to capacity, by providing level 3 care to moderately symptomatic patients, who may require high-flow oxygen, nursing care, and daily living assistance. 3) the acute care model refers to capability building by providing step-down (level 2) or ICU care (level 1) [15]. The NMC-FED does not exclusively fit into one of these models; it could provide level 4 care to patients who have underlying medical conditions, and level 3 care to a certain extent, in addition to level 5 care. It could also provide cardiopulmonary resuscitation and quickly transfer patients in return of spontaneous circulation to the NMC main hospital. Thus, it differs from the Korean CTC model, where only level 5 care could be provided, which is far from oxygen therapy and cardiopulmonary resuscitation; CTCs can be operated remotely by dispatching a minimal number of medical staff and conducting monitoring via telemedicine. For example, a university hospital operated one CTC located 153 kms away [8], while three different tertiary hospitals in Seoul operated other CTCs located 75 kms, 190 kms, and 225 kms away, respectively, at the epicenter of Daegu [11]. Although only 3% of the patients were transferred to nearby hospitals [10], the continuity of care could be disrupted in this situation.
Similar to the US State Island University Hospital East (SIUH-E), the NMC-FED had advantages in providing care with continuity [3]. It cared for patients, who were stable but not ready for discharge and were transferred from the main hospital; the seamless integration of systems (for example, electronic medical records, prescription, and laboratory tests) and physical proximity to the main hospital were its distinctive features.
Another characteristics is that the NMC-FED considered the health equity, prioritizing the vulnerable population in need of medical and social care. For example, the residents in long-term care facilities, homeless shelters, group homes, or detention facilities, who could not be discharged to their original residences without negative test results were cared for in the NMC-FED. Particularly, those in need of augmented security could receive proper medical services; one building was physically separated from the others (Figure 1, Building C) and the entire perimeter of the site is guarded by the Ministry of National Defense. Similar mission was found in a “long-term acute care hospital” organized in Boston, to provide the post-acute care services to COVID-19 patients whom skilled nursing facilities could not afford. A considerable proportion of patients were among the disadvantaged population, including shelter residents, immigrants, and the uninsured [16]. The NMC-FED features are consistent with the recommendations suggesting that ACF-related decisions should be based on local contexts [15].
Most ACFs were quickly converted from existing public structures, such as an old newspaper company building [14], a psychiatric facility yet to open [3], convention centers [1, 17], and a gymnasium [18], and operated in a limited time of medical surges. For example, in Wuhan city, about 4,000 beds were made within 29 hours and 16 hospitals with 13,000 beds were constructed in the following 3 weeks; these Fangcang shelter hospitals provided care to 12,000 patients [4]. Korean CTC models that make use of dormitories could also function immediately. In the first wave of the outbreak, more than 3,000 patients (one-third of the total cases) were cared for in the CTCs [8]. However, it usually takes time for planning and construction of ACFs, and strong non-pharmaceutical interventions are adopted in parallel to mitigate medical surges. Many ACFs could not provide timely services as expected, due to a significant time gap between the surge and the actual functioning of the ACFs. For example, the Philadelphia facility, converted from a gymnasium over the course of 3 weeks, could only care for 14 patients in the next 10 days [18]. For these reasons, ACFs should be maintained as a “warm site” to immediately respond to the outbreak even after the medical surge subsides [15]. The NMC-FED determined to maintain its function as a warm site in the planning stage, with a long-term orientation, and it could cope with the persistent demands even after calming down of the third-wave epidemic.
Over the course of planning and construction, the NMC-FED was faced with various challenges such as construction, workforce, care flow and emergency responses, patient safety, and logistics. Innovative solutions and improvisations were made to meet the standards of infection prevention and control, and to provide care to patients without significant compromise. Physical layout, staffing, patient care, and facility operation were modified for this purpose, as shown in Table 4. Also, the admission criteria could not be strictly applied in the field, where patients varied in their social and medical needs and availability of other facilities were limited; for example, the NMC-FED accommodated 5 patients older than 75 years, on the judgement of the medical director. Although our experience cannot be exactly replicated in different contexts, they could inform others, who aim to implement an ACF to cope with medical surges in public health emergencies.
Notes
Funding
This research was supported by Public Health Research Program funded by the National Medical Center (grant No. NMC2020-PR-06)
DISCLOSURES
The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION
Conceptualization: Sung HK, Kim MH, Min HS, Chung KH. Methodology: Sung HK, Kim MH, Min HS. Formal analysis: Sung HK, Min HS, Lee B. Data curation: Chin BS, Sung HK, Min HS, Lee B Writing - original draft preparation: Sung HK, Kim MH. Writing - review and editing: Chin BS, Koh IS, Chung KH. Approval of final manuscript: all authors.



