COVID-19 pandemic and its impact on health expenditure
Article information
Abstract
Purpose
The large-scale spread of COVID-19 has led to a burden on the national healthcare financial system. This study assessed the medical cost of COVID-19 hospitalizations and its effect on national health expenditures in Korea and investigated the factors that affected the cost of hospitalization for COVID-19 patients.
Methods
A total of 23,812 COVID-19 patients were reported as of September 30, 2020. 18,854 cases of COVID-19 hospitalization were claimed by The Health Insurance Review and Assessment Service with a total of 14,283 inpatients.
Results
From January to September 2020, the total cost of treatment for hospitalized COVID-19 patients in Korea was 79,277,000 USD. The mean cost per case was 4,284 USD (IQR, 649-5,257). Medical costs were high in the elderly, those with severe symptoms, medical aid beneficiaries, and those who died during treatment. The mean length of hospital stay of COVID-19 patients was 17.3 days (IQR 9-23) and was high in women, the elderly, medical aid beneficiaries, and patients in Daegu and Gyeongsangbuk provinces. The differences in medical costs between sex, age, insurance, region, treatment result, and length of stay groups according to severity were significant for all variables. Moreover, the mean costs per case and per day were higher in medical aid beneficiaries than those subscribed to health insurance (P<.05).
Conclusions
In Korea, the medical cost for treatment of COVID-19 patients was low compared to that of other countries, as well as the treatment cost for the H1N1 influenza in Korea. Factors affecting the medical cost of COVID-19 treatment included age, severity, type of insurance, and treatment results. Additional follow-up studies that also include the cost of screening and quarantine in the analysis of medical costs are necessary.
Introduction
Coronavirus Disease-19 (COVID-19) is an emerging infectious disease that has caused tremendous socio-economic damage, with approximately 170 million cases of infection and 35 million deaths worldwide as of May 24, 2021 [1]. The COVID-19 pandemic has led to a physical and financial burden on the health care system of every country around the world. Approximately 20% of COVID-19 patients require inpatient treatment, and 5%–30% of these inpatients need intensive care [2-4], leading to increased medical costs and demand for hospital beds. Spain has spent an additional €3.9 billion on its health care system in response to the COVID-19 pandemic [5], with the mean cost of direct treatment per COVID-19 patient being greater than 3,000 US dollars (USD) in several countries [6,7], which is 4-5.5 times higher than that of other infectious diseases such as influenza and pertussis [7].
In Korea, the first confirmed case of COVID-19 infection occurred on January 20, 2020. Since then, 122,634 confirmed cases and 1,831 deaths have been reported, as of May 24, 2021 [8], and the Korean government has implemented a 3T strategy of active testing, tracing, and treatment from the start of the outbreak to identify, isolate, and treat infected patients to effectively prevent the spread of COVID-19 and ensure the smooth functioning of the medical system. The government paid for the cost of testing and treatment of COVID-19, reducing the financial burden of hospitalization on the patients [9]. As such, Korea has responded to the COVID-19 pandemic in a relatively stable manner compared to other countries; however, the burden on the medical system continues with numerous COVID-19 cases being reported daily. Furthermore, as experts predict COVID-19 to become endemic [10], over the long term, it is necessary to analyze the impact of COVID-19 on the health care system and seek effective countermeasures. In particular, as the cost of COVID-19 treatment is high in other countries, it is necessary to assess the treatment cost of COVID-19 in Korea, where the medical cost is fully covered by the government, especially for cases of hospitalization that require great expenditure of resources.
This study assessed medical costs due to hospitalization for COVID-19 and its effect on national health expenditure in Korea and investigated factors that affected the cost of hospitalization for COVID-19 patients.
Methods
Study Design, Setting, and Population
This retrospective, observational study analyzed the total cost of hospitalization related to COVID-19 in Korea. COVID-19 patient management data from the Korea Disease Control and Prevention Agency Centers and Health Insurance Review and Assessment Service (HIRA) health insurance claim data were linked together in this study. Clinical information such as severity, symptoms, and treatment progression of COVID-19 patients was managed in the patient management database of the Korea Disease Control and Prevention Agency, and data on claims for diagnosis and medical treatment were managed by HIRA. In Korea, all COVID-19 related medical costs including hospital fees, tests, and treatment, are paid for by health insurance and can be found in the HIRA claim data. A total of 23,812 patients who tested positive for the COVID-19 Real time reverse transcription polymerase chain reaction (rRT-PCR) test were extracted from January 1 to September 30, 2020. Among these patients, 15,083 patients who claimed medical costs related to COVID-19 more than once were selected, including 14,598 inpatients. Those who had missing variables or who were repeatedly hospitalized were excluded, and 14,283 patients were included in the final analysis.
Data collection
Sex, age, insurance type, length of stay, and medical cost of the participants were extracted from the HIRA claims data. The age groups of the participants were divided into groups of 1) 0 through 19 years; 2) 20 through 29 years; 3) 30 through 39 years; 4) 40 through 49 years; 5) 50 through 59 years; 6) 60 through 69 years; 7) 70 years or more. The length of stay was calculated as the difference between the start and end dates of treatment for those with COVID-19 diagnosis codes (KCD U07.1, U07.2). Medical costs were grouped into consultation fees, cost of laboratory tests, cost of procedures and surgeries, hospital room cost, and bundled payment for long-term care, hospice, and mental diseases. Information regarding the region of residence, treatment results, and severity of the disease were obtained from the patient management database. The region of residence was divided into Seoul metropolitan area, Daegu and Gyeongsangbuk provinces, and other areas according to COVID-19 endemic regions [9]. The treatment result was divided into recovered and expired. The severity of the patients’ condition in the last hospitalization was assessed based on blood pressure, pulse rate, respiratory rate, and body temperature obtained by local government epidemiological investigators before hospitalization. For those participants who could not undergo physical examination, the severity of disease was divided into five levels: 1) asymptomatic, 2) mild, 3) moderate, 4) severe, and 5) very severe, based on age, consciousness, underlying diseases, smoking, and high fever.
Statistical analysis
Descriptive statistics were used to present the general characteristics, length of stay, and medical cost of the participants using frequency, percentage, and interquartile range (IQR). The mean length of stay was calculated by dividing the total days of stay by the number of hospitalizations and was expressed as the mean and quartiles. The medical cost, the total cost of treatment, cost per case of hospitalization (total cost of treatment divided by the number of hospitalizations), and cost per day of stay (total cost of treatment divided by the number of hospitalized days) were calculated and expressed as mean and quartiles.
The Cochran-Mantel-Haenzel test was conducted to assess the difference in the number of patients according to the severity of the disease. In addition, a two-way ANOVA was conducted to assess the differences in the mean treatment cost according to severity. All tests were two-sided, and a P-value of less than .05, was considered statistically significant. The SAS Enterprise guide 7.15 program was used for all statistical analyses.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of the Health Insurance Review and Assessment Service (2020-106-001).
Results
Characteristics of COVID-19 patients
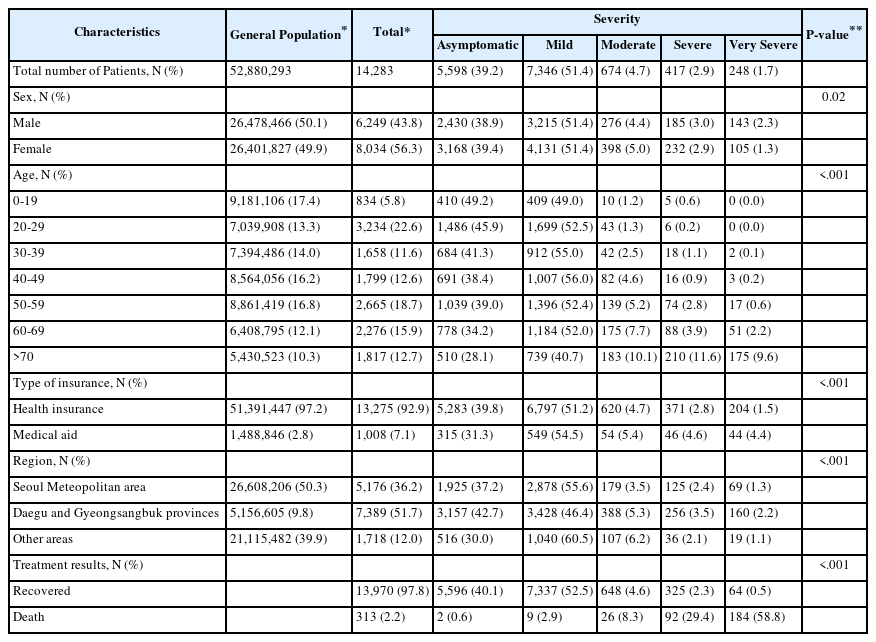
As of September 30, a total of 14,283 patients were hospitalized for COVID-19 in Korea, including 8,034 (56.3%) female patients. The number of female patients was greater than the number of male patients (6,249; 43.8%), and the proportion of female patients was higher than the proportion of females in the general population. The highest number of patients hospitalized for COVID-19 were between the ages of 20 and 29 (22.6%), followed by those between the ages of 50 and 59 (18.7%). The proportion of patients aged 20 to 29 and older than 50 years was higher in the patient group than in the general population. A total of 13,275 (92.9%) patients hospitalized for COVID-19 had health insurance, and 1,008 (7.1%) patients were medical aid beneficiaries. The ratio of COVID-19 patients with medical aid benefits was higher than the ratio of beneficiaries in the general population (2.8%). More than half of the COVID-19 patients (7,389 patients; 51.7%) were from Daegu and Gyeongsangbuk provinces, and the ratio of COVID-19 patients from Daegu and Gyeongsangbuk provinces was higher than the ratio of people from Daegu and Gyeongsangbuk in the general population. Of the total patients, 13,970 (97.8%) recovered and were discharged, while 313 (2.2%) died. Of the total patients, 5,598 (39.2%) were asymptomatic, while 7,346 (51.4%) patients showed mild symptoms. The ratio of asymptomatic (38.9% vs. 39.4%) and mildly symptomatic (51.4% vs. 51.4%) patients were similar in both men and women, and more men were in the very severe group (2.3% vs. 1.3%, p=0.02). Young patients were mostly asymptomatic or showed mild symptoms. As age increased, the number of patients with severe and severe symptoms increased. In particular, 210 (11.6%) and 175 (9.6%) patients aged > 70 years showed severe and very severe symptoms, respectively. A greater number of patients with medical aid showed severe (2.8% vs. 4.6%) and very severe (1.5% vs. 4.4%) symptoms compared to those who subscribed to health insurance. In addition, most of the patients who died were in the severe (29.4%) or very severe (58.8%) groups.
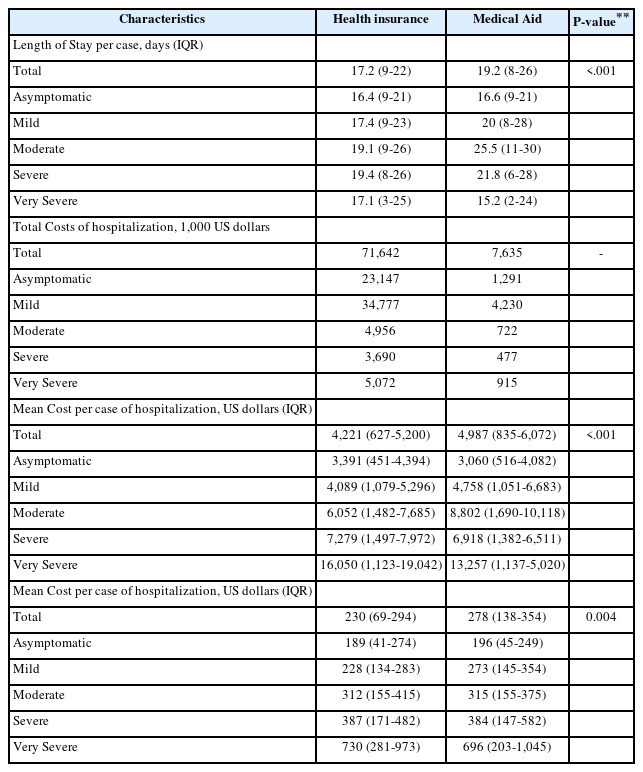
Length of hospital stay and medical cost
The mean length of stay for all COVID-19 patients was 17.3 days (IQR 9-23), and the total cost of hospitalization for COVID-19 patients was 79,277,000 USD. The mean cost per case was 4,284 USD (IQR, 649-5,257). The mean cost per case was 4,642 USD (IQR 766-5,585) for men, which was higher than the 4,003 USD (IQR 588-5,007) for women. The mean length of stay, total cost, and mean cost per case increased with age. In the patient group aged < 19 years, the mean length of stay and mean cost per case were 15.5 days (IQR 9-19) and 3.068 USD (IQR 1553-4,112), respectively, which was significantly different from that in patients over the age of 70 (mean length of stay: 21.1 [IQR 9-28] and mean cost per case 7,172 USD [IQR 1,763-8,223]). The mean cost per case was 4,221 USD (IQR 627-5,200) for national health insurance subscribers, which was higher than 4,987 USD (IQR 835-6,072) for medical aid beneficiaries. The mean length of stay for patients in Daegu and Gyeongsangbuk provinces was 18.1 (IQR 9-23), which was higher than that of patients in other regions. However, patients in Daegu and Gyeongsangbuk provinces had the lowest mean cost per case at 3,465 USD (IQR 433–4,067). The mean length of stay was shorter for patients who recovered than for those who died (IQR 17.4 vs. 14.8%); however, the mean cost per case was greater for patients who recovered (4,117 USD, IQR 622-5,209 vs 10,999, IQR 1,266-10,227). The mean length of stay and mean cost per case tended to increase with the severity of symptoms, except in those with very severe symptoms. The mean cost per day for all patients was 234 USD (71-299 USD) and increased with the severity. The mean cost per day for those with very severe symptoms was 724 USD (IQR 279-980), which was more than 3.5 times higher than that of asymptomatic patients.
The mean cost per case was compared based on patient severity. Regardless of the severity, the mean cost per case was higher in men than in women (P=0.04) and with age. The mean cost per case was 3,068 USD (IQR 553-4,112) for those between the ages of 0 and 19 and 7,172 USD (IQR 1,763-8,223) for those over the age of 70. A similar trend was observed in all severity groups. However, in the very severe group, the mean cost per case was 12,723 USD (IQR–1,147-11,314) for those over the age of 70, which was lower than that of those aged 40-49, 50-59, and 60-69 (p<0.001). The mean cost per case for national health insurance subscribers was 4,221 USD (IQR 627-5,200), which was lower than the 4,987 USD (IQR 835-6,072) of medical aid beneficiaries. However, the mean cost per case was lower in the asymptomatic, mild, and very severe groups. In all severity groups, excluding the very severe group, the mean cost per case was the lowest for patients in Daegu and Gyeongsangbuk provinces. In the very severe group, the mean cost per case was highest for patients in Daegu and Gyeongsangbuk provinces (P<0.001). The mean cost per case was higher in patients who died in the asymptomatic, mild, and severe groups. In contrast, in the moderate and very severe groups, the mean cost per case was higher in the patients who recovered (P<0.001). In all severity groups, a longer length of stay was associated with an increased mean cost per case (P<0.001).
The medical costs of COVID-19 were further analyzed in detail. Hospital room cost accounted for the greatest portion of total medical costs, followed by the cost of laboratory tests, cost of procedure and surgery, and consultation fees. As the age of the patients increased, the proportion of hospital room costs decreased, while the proportion of the cost of procedure and surgery increased. The cost of procedure and surgery accounted for 12.9% of the total medical cost of patients with medical aid, which was higher than 7.7% of the total medical cost of patients subscribed to health insurance. In addition, the proportion of the cost of procedure and surgery was higher in patients from the Daegu and Gyeongsangbuk regions than in patients from other regions. For those patients who died, the cost of procedure and surgery accounted for 41% of the total medical cost and was higher than the hospital room cost of 34%. The proportion of the cost of the procedure and surgery tended to increase with the severity.
Compared to health insurance subscribers and medical aid beneficiaries, the total medical cost was higher in those with health insurance than in those with medical aid (71,642,000 vs. 7,635,000 USD). However, the mean cost per case (4,221 USD, IQR 627-5,200 vs 4,987 IQR 835-6,072) and mean cost per day (230 USD, IQR 69-294 vs. 278 IQR 138-354) were higher in those with medical aid. When patients were analyzed according to severity, the length of stay was greater in medical aid recipients than in health insurance beneficiaries (17.2, IQR 9-22 vs. 19.2; IQR 8-26).
Discussion
This study assessed the total medical costs of patients hospitalized with COVID-19 and investigated the factors affecting medical costs, using national health insurance data. As of September 30, 2020 in Korea, 14,283 patients were hospitalized for COVID-19, and the total medical cost for hospitalization was 79,277,000 USD. The mean cost per case of hospitalization was 4,284 USD (IQR: 649 – 5,257). Medical costs increased with age, severity, for medical aid beneficiaries, and for cases of death.
The cost of hospitalization treatment in Korea is lower than that of China, where the mean cost per case and total medical cost is approximately 3,192–6,827 USD and 494,202,120 USD, respectively [11,12]. In addition, the mean cost per case in Korea was only 1/10 of that in the US (43,986 USD) [13]. The mean cost of treatment of COVID-19 in Korea until September 30 was only 0.4% of the total cost of hospitalization (21 billion USD), which did not have significant financial effects on the Korean healthcare system. There is a lot of concern regarding the growing medical and non-medical financial burden due to COVID-19. In the United States, medical costs have increased by 30%–40% following the outbreak of COVID-19 [14], and there are concerns about how long the costs will continue to increase and affect the GDP. Although the medical cost varies between countries, the low financial burden for the treatment of COVID-19 patients may be related to the COVID-19 response strategies of Korea. Korea has implemented a 3T (test, trace, and treat) strategy to delay the spread of COVID-19 from the early stage and "flatten the curve" of COVID-19 patients through rapid large-scale examination and follow-up, early hospitalization, and treatment of those who were in contact with infected patients [16]. As a result, early detection, treatment, and hospitalization of COVID-19 patients before the onset of severe symptoms would have lowered the resulting hospitalization cost.
Compared to the medical cost of treating the H1N1 influenza, a pandemic that occurred in Korea in 2009, the financial impact of COVID-19 on medical system has been relatively low. The total cost of hospitalization for H1N1 influenza in Korea was 77 million USD, the mean cost per case was 625.8 USD [17]. The total number of H1N1 influenza-infected patients was approximately 3 million, and the H1N1 influenza treatment cost accounted for 1.24% of the total medical cost in 2009, which imposed a greater financial burden than COVID-19.
The mean cost per case for COVID-19 (4,284 USD) and mean cost per case for very severe patients (15,560 USD) was 2.4 times and 8.8 times higher than the mean cost per hospitalization (1,759 USD), respectively [19]. Thus, a long-term epidemic of COVID-19 and an increase in the number of patients could burden medical costs. In particular, we observed that treatment costs increase significantly in patients with very severe symptoms, which is consistent with a previous study conducted in China [12]. Therefore, early detection and treatment of patients before the onset of severe symptoms, may be a strategy to reduce medical costs.
In our study, medical aid recipients had a high length of stay and mean cost per case. A previous study demonstrated that medical aid recipients had a higher prevalence and fatality rate of COVID-19 and more underlying diseases than the health insurance beneficiaries [9]. Therefore, it is thought that underlying diseases may have influenced the higher severity of disease in medical aid recipients. However, medical aid recipients had a longer length of stay and mean cost per case in the same severity groups. Therefore, further data collection and analysis are necessary. Patients in Daegu and Gyeongsangbuk provinces showed a lower mean cost per case compared to patients in other regions. In all severity groups, excluding the very severe group, patients from Daegu and Gyeongsangbuk provinces had a lower mean cost per case. This may be attributed to the large number of young patients in those provinces.
Several limitations must be considered when interpreting the findings of this study. First, only patients who were confirmed to have COVID-19 over the course of September 2020 were included in the analysis. Thus, the analysis period was relatively short. In Korea, more than 10,000 confirmed cases of COVID-19 were reported monthly, as of December 2020, and the trend in medical costs may vary. Second, there were differences between the date of medical treatment of patients and the date of final medical cost claims by the medical institutions. Thus, medical costs may have been underestimated. Further accumulation of medical cost claims data would help to better estimate the mean cost per case. Third, only the cost of hospitalization treatment was analyzed in this study. However, to evaluate the financial burden, a comprehensive analysis of the costs inside and outside the hospital, for screening and quarantine to find patients, as well as social costs due to loss of productivity, is necessary. Follow-up studies are necessary for further data collection and analysis. Despite these limitations, this study is meaningful as it used Korea's national health insurance data to assess the medical cost of treatment of COVID-19 in order to investigate the financial burden placed by COVID-19. As long as the COVID-19 pandemic persists, various efforts to reduce medical costs need to be continued.
Notes
Funding: This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
DISCLOSURE
All authors have no potential conflicts of interest.